glioblastoma
 Glioblastoma multiforme (GBM WHO grade IV) is the most commonly occurring and most malignant brain tumour, characterised by extensive infiltration of the brain. Although there is no clear explanation as to what causes a GBM, certain genetic predispositions do appear to play a role, and prior exposure of the brain to ionising radiation has been associated with significantly higher rates of occurrence of gliomas.
Glioblastoma multiforme (GBM WHO grade IV) is the most commonly occurring and most malignant brain tumour, characterised by extensive infiltration of the brain. Although there is no clear explanation as to what causes a GBM, certain genetic predispositions do appear to play a role, and prior exposure of the brain to ionising radiation has been associated with significantly higher rates of occurrence of gliomas.
The prognosis of GBM is unfortunately uniformly poor, and treatment is therefore centred primarily on maintenance of quality of life. First diagnosis is not unusually made when the tumour has already reached significant proportions, as it is often the case that patients become symptomatic only then. Without treatment, survival is typically up to three months from the time of diagnosis. With optimal multi-
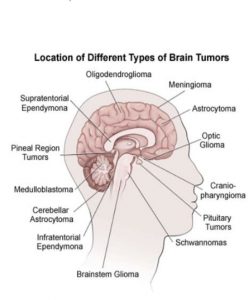
A GBM may be primary, when it is arising directly as a Grade IV glioma, or secondary, arising from a Grade II or III glioma. Primary GBM develops more commonly in older patients, while secondary GBM develops more commonly in younger patients. Although the majority of GBM cases are registered from the fourth decade of life onwards, brainstem GBM is a paediatric malignancy, occurring most often in the very young. The time taken for progression from a lower grade glioma to a GBM is variable, ranging from several months to more than a decade, with a mean interval of about 5 years.
The current treatment strategy consists of maximum possible reduction of tumour bulk without causing fresh neurological deficit, followed by combined radio-
 Adjuvant treatment is aimed to start in a time frame around 4 weeks after surgery, assuming the underlying clinical condition allows the start of the combined modality treatment with radiotherapy and chemotherapy. Given that any remaining tumour after an operation can still grow after the commencement of radiotherapy/chemotherapy, it is not uncommon to see in some patients an increase in the residual tumour size at the 1st post-
Adjuvant treatment is aimed to start in a time frame around 4 weeks after surgery, assuming the underlying clinical condition allows the start of the combined modality treatment with radiotherapy and chemotherapy. Given that any remaining tumour after an operation can still grow after the commencement of radiotherapy/chemotherapy, it is not uncommon to see in some patients an increase in the residual tumour size at the 1st post-
Careful surveillance with serial MRI scans is a crucial part of medical care, because tumour regrowth requires alteration of current treatment or, for patients in the observation phase, restarting treatment.
A regime for combined radio-
Radiation:
Tumour site along with a security margin: 30 sessions at the rate of 2Gy per fraction for 5 days/week (60Gy in total).
Chemotherapy:
Temozolomide: Concurrent period with radiotherapy: from Day 1-
Four weeks break (Day 70)
Temozolomide: Maintenance period from day 71 (Cycle1): only 5 days per month, every 28 days for 6 months (Cycle 6), at the rate of 150mg/m2 for the first cycle, increased to 200mg/m2 with the second cycle and onward.
Considering treatment with Temozolomide causes suppression of the bone marrow, a blood count is checked regularly during the period of combined radio-
Recurrences are usually local at the site of first occurrence, or sometimes in other areas of the brain. The treatment of recurrences needs to be tailored to the individual case, keeping the patient’s general condition in perspective, because of the possible risk of iatrogenic neurotoxicity. Besides best supportive care if the performance status (PS) is poor, repeated surgery in the case of local GBM or for symptomatic large lesions can be an option as well as systemic chemotherapy with, for example, TMZ, Lomustine, PCV, bevacizumab, platinum based regimens and Cyclophosphamide. It is also possible to consider re-
Another option for patients with recurrent high grade gliomas is re-irradiation, even if it is to a site previously irradiated.
